Abstract
Background
The efficacy of Bendamustine and Rituximab (BR) for indolent NHL (iNHL) has been demonstrated in 2 randomised studies (StiL NHL1 and BRIGHT), although combination therapy with monoclonal antibodies remains an off-label use. Increased toxicity was apparent in both bendamustine cohorts of the GALLIUM study, with 5% treatment-related mortality (TRM) versus 1.8% in the CHOP/CVP arms. Recently, the UK MHRA (Medicines and Healthcare products Regulatory Agency) issued notification of increased infection risks in the context of bendamustine combination therapy. Given these concerns we undertook an observational analysis of T-cell reconstitution and mortality following Bendamustine-based therapy within a large University hospital.
Methods
Patients who received bendamustine for CLL or lymphoma between April 2012-Jan 2017 were identified from our electronic prescribing database. We evaluated clinical outcomes following treatment, and assessed absolute lymphocyte count (ALC), CD4, CD8, NK-cells and immunoglobulin levels over time.
Results
173 patients were identified, 171 (99%) received bendamustine combination therapy, 2 (1%) received monotherapy. The median age was 68 years (range 34-93). 71% had iNHL (follicular n=63, marginal zone n=34, LPL n=25), 22% had CLL whilst mantle, DLBCL and Hodgkin lymphoma accounted for 7% (n=13). The median number of previous therapy lines was 1 (0-7). Excluding CLL and overt leukaemic disease (32% of the cohort), the median ALC pre-bendamustine was 1.3x109/l (0.2-3.9x109/l) with a median nadir at 1 month post treatment of 0.5x109/l. After 12 months, 77% of this cohort had an ALC of ≥ 0.5 x109/l and 28% an ALC of ≥ 1.0 x109/l . 82 patients (47%) had immunoglobulin levels assessed within 3-12 months of bendamustine with a median IgG level of 5.2g/l (range 2-14.3). Of these 38 (46%) were <5g/l, and 15 (18%) were <3g/l.
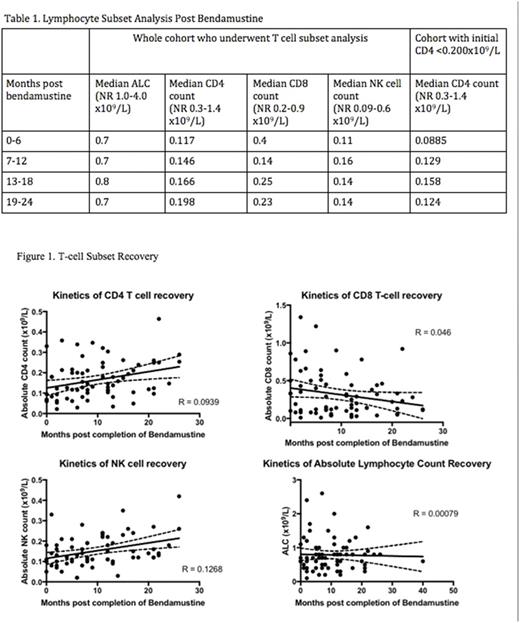
Given the potential unreliability of ALC in the context of iNHL and CLL and to better inform duration of antimicrobial prophylaxis, we evaluated T- lymphocyte recovery in more detail. Of the whole cohort, 27% (n=47) had undergone a full lymphocyte subset analysis by flow cytometry at least once following bendamustine-based treatment. The median number of lymphocyte subset analyses evaluated per patient was two (range 1-5) at time-points ranging from 1-40 months post-bendamustine.
The median CD4 count in the first 6 months post bendamustine was 0.117 x109/L. 30 patients (65%) had at least one CD4 count <0.200 x109/L (200/ul), and these patients had an initial median CD4 count of 0.085 x109/L. We observed a marked delay in CD4 recovery for the whole cohort and those with initial post treatment CD4 count <0.200 x109/L, with median CD4 counts at 24 months of 0.198 x109/L and 0.124 x109/L respectively (table 1). NK-cell numbers on the same follow-up samples were also depleted, with 21% initially below the lower limit of normal, and although less profound reductions in absolute numbers were seen, recovery followed similar kinetics to CD4 cells. Interestingly, median CD8 counts were within normal range in the first 6 months post bendamustine treatment, with no clear change in absolute numbers over time (figure 1).
For the whole cohort, 31 deaths were observed (18%), 11 due to progressive disease. Of the 20 non-lymphoma-related deaths, 10 were due to infection but only 4 (13%) occurred within 6 months of bendamustine. Of the remaining 6 deaths, all had received at least 1 subsequent line of treatment (including stem cell transplant in 3 cases). Of the remaining 10, 4 occurred within 12 months of bendamustine and were attributed to lung fibrosis, glioblastoma, gastric cancer and pulmonary embolism.
Conclusion
Amongst a population-based cohort of bendamustine-treated patients, we have demonstrated slow kinetics of T-cell reconstitution. The majority of patients experienced marked CD4 lymphopenia, with most failing to reconstitute >0.200 x109/L by 24 months post therapy. Similar but less profound reductions were seen in NK-cell numbers in addition to clinically significant reductions in IgG levels. Importantly, ALC did not correlate with the CD4 numbers and is unlikely to be a reliable indicator of T-cell recovery. These data may, at least in part, explain the TRM of bendamustine-based therapy and supports extended duration of antimicrobial prophylaxis against opportunistic infection, informed by CD4 recovery.
McMillan: Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel sponsorship. Bishton: Roche: Other: Travel Sponsorship. Fox: AbbVie: Consultancy, Honoraria, Other: Travel Sponsorship, Research Funding; Roche: Consultancy, Honoraria, Other: Travel Sponsorship, Research Funding, Speakers Bureau; Janssen: Consultancy, Honoraria, Other: Travel Sponsorship, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal